Online Newsletter Committed to Excellence in the Fields of Mental Health, Addiction, Counseling, Social Work, and Nursing
Showing posts with label brain. Show all posts
Showing posts with label brain. Show all posts
December 01, 2014
High-fructose diet in adolescence may exacerbate depressive-like behavior
What do you think of this article?
"Animal study shows that diet alters important pathways associated with brain's response to stress
The consumption of a diet high in fructose throughout adolescence can worsen depressive- and anxiety-like behavior and alter how the brain responds to stress, according to new animal research scheduled for presentation at Neuroscience 2014, the annual meeting of the Society for Neuroscience and the world's largest source of emerging news about brain science and health.
"Our results offer new insights into the ways in which diet can alter brain health and may lead to important implications for adolescent nutrition and development," said lead author Constance Harrell of Emory University in Atlanta.
Harrell is presenting her work Saturday, Nov. 15, Halls A-C, 3-4 pm and participating in an "Unhealthy diet, unhealthy mind"-themed press conference on Tuesday, Nov. 18 at 12:30 pm.
Harrell is a graduate student working with Gretchen Neigh, PhD, assistant professor of physiology, psychiatry and behavioral sciences at Emory University School of Medicine.
Fructose, a sugar found naturally in fruits and vegetables but also added to many processed foods and beverages, can promote negative cardiovascular effects. It also stimulates neural pathways that affect how the brain responds to stress, which can have important behavioral effects, including the worsening of symptoms related to depression and anxiety. Such effects are of particular concern during the teen years, which is a critical time for the development of the brain's stress response.
To determine whether fructose consumption has the potential to create long-term changes in metabolism and behavior during adolescence, Harrell and her colleagues gave both adolescent and adult rats either a standard or a high-fructose diet. After 10 weeks, the adolescent but not adult rats on the high-fructose diet had a different stress hormone response to an acute stressor, which was consistent with their depressed-like behavior. A genetic pathway in the brain that plays a key role in regulating the way the brain responds to stress was also altered. These findings indicate that consuming a diet high in fructose throughout adolescence may exacerbate depressive behaviors and affect the way the body and the brain respond to stress."
###
For more mental health topics and Continuing education in 3 easy steps, please visit Online MFT Continuing Education
Labels:
behavior,
behavioral,
brain,
depressive,
fructose,
online mft continuing education,
stress
October 20, 2014
Mental Rest and Reflection Boost Learning, Study Suggests
What do you think of this article supported by the NIH and published by University of Texas at Austin?:
"The patterns of brain activity recorded in this fMRI scanner revealed how mental rest and reflection on past learning activities can boost future learning. Photo credit: Jeff Luci.
AUSTIN, Texas — A new study, which may have implications for approaches to education, finds that brain mechanisms engaged when people allow their minds to rest and reflect on things they've learned before may boost later learning.
Scientists have already established that resting the mind, as in daydreaming, helps strengthen memories of events and retention of information. In a new twist, researchers at The University of Texas at Austin have shown that the right kind of mental rest, which strengthens and consolidates memories from recent learning tasks, helps boost future learning.
The results appear online this week in the journal Proceedings of the National Academy of Sciences.
Margaret Schlichting, a graduate student researcher, and Alison Preston, an associate professor of psychology and neuroscience, gave participants in the study two learning tasks in which participants were asked to memorize different series of associated photo pairs. Between the tasks, participants rested and could think about anything they chose, but brain scans found that the ones who used that time to reflect on what they had learned earlier in the day fared better on tests pertaining to what they learned later, especially where small threads of information between the two tasks overlapped. Participants seemed to be making connections that helped them absorb information later on, even if it was only loosely related to something they learned before.
"We've shown for the first time that how the brain processes information during rest can improve future learning," says Preston. "We think replaying memories during rest makes those earlier memories stronger, not just impacting the original content, but impacting the memories to come.
Until now, many scientists assumed that prior memories are more likely to interfere with new learning. This new study shows that at least in some situations, the opposite is true.
"Nothing happens in isolation," says Preston. "When you are learning something new, you bring to mind all of the things you know that are related to that new information. In doing so, you embed the new information into your existing knowledge."
Preston described how this new understanding might help teachers design more effective ways of teaching. Imagine a college professor is teaching students about how neurons communicate in the human brain, a process that shares some common features with an electric power grid. The professor might first cue the students to remember things they learned in a high school physics class about how electricity is conducted by wires.
"A professor might first get them thinking about the properties of electricity," says Preston. "Not necessarily in lecture form, but by asking questions to get students to recall what they already know. Then, the professor might begin the lecture on neuronal communication. By prompting them beforehand, the professor might help them reactivate relevant knowledge and make the new material more digestible for them."
This research was conducted with adult participants. The researchers will next study whether a similar dynamic is at work with children.
This work was supported by the National Institute of Mental Health of the National Institutes of Health, the National Science Foundation (NSF) through the NSF CAREER Award and the Department of Defense through the National Defense Science and Engineering Graduate Fellowship Program."
For more information on mental health topics, please visit CEUs for Counselors
Labels:
brain,
ceus for counselors,
learning,
mental,
mental health,
process,
relaxation,
rest,
thinking
July 23, 2014
Seeing the inner workings of the brain made easier by new technique from Stanford
What do you think about this article?
"Last year Karl Deisseroth, a Stanford professor of bioengineering and of psychiatry and behavioral sciences, announced a new way of peering into a brain – removed from the body – that provided spectacular fly-through views of its inner connections. Since then laboratories around the world have begun using the technique, called CLARITY, with some success, to better understand the brain's wiring.
However, Deisseroth said that with two technological fixes CLARITY could be even more broadly adopted. The first problem was that laboratories were not set up to reliably carry out the CLARITY process. Second, the most commonly available microscopy methods were not designed to image the whole transparent brain. "There have been a number of remarkable results described using CLARITY," Deisseroth said, "but we needed to address these two distinct challenges to make the technology easier to use."
In a Nature Protocols paper published June 19, Deisseroth presented solutions to both of those bottlenecks. "These transform CLARITY, making the overall process much easier and the data collection much faster," he said. He and his co-authors, including postdoctoral fellows Raju Tomer and Li Ye and graduate student Brian Hsueh, anticipate that even more scientists will now be able to take advantage of the technique to better understand the brain at a fundamental level, and also to probe the origins of brain diseases.
This paper may be the first to be published with support of the White House BRAIN Initiative, announced last year with the ambitious goal of mapping the brain's trillions of nerve connections and understanding how signals zip through those interconnected cells to control our thoughts, memories, movement and everything else that makes us us.
"This work shares the spirit of the BRAIN Initiative goal of building new technologies to understand the brain – including the human brain," said Deisseroth, who is also a Stanford Bio-X affiliated faculty member.
Eliminating fat
When you look at the brain, what you see is the fatty outer covering of the nerve cells within, which blocks microscopes from taking images of the intricate connections between deep brain cells. The idea behind CLARITY was to eliminate that fatty covering while keeping the brain intact, complete with all its intricate inner wiring.
The way Deisseroth and his team eliminated the fat was to build a gel within the intact brain that held all the structures and proteins in place. They then used an electric field to pull out the fat layer that had been dissolved in an electrically charged detergent, leaving behind all the brain's structures embedded in the firm water-based gel, or hydrogel. This is called electrophoretic CLARITY.
The electric field aspect was a challenge for some labs. "About half the people who tried it got it working right away," Deisseroth said, "but others had problems with the voltage damaging tissue." Deisseroth said that this kind of challenge is normal when introducing new technologies. When he first introduced optogenetics, which allows scientists to control individual nerves using light, a similar proportion of labs were not initially set up to easily implement the new technology, and ran into challenges.
To help expand the use of CLARITY, the team devised an alternate way of pulling out the fat from the hydrogel-embedded brain – a technique they call passive CLARITY. It takes a little longer, but still removes all the fat, is much easier and does not pose a risk to the tissue. "Electrophoretic CLARITY is important for cases where speed is critical, and for some tissues," said Deisseroth, who is also the D.H. Chen Professor. "But passive CLARITY is a crucial advance for the community, especially for neuroscience." Passive CLARITY requires nothing more than some chemicals, a warm bath and time.
Many groups have begun to apply CLARITY to probe brains donated from people who had diseases like epilepsy or autism, which might have left clues in the brain to help scientists understand and eventually treat the disease. But scientists, including Deisseroth, had been wary of trying electrophoretic CLARTY on these valuable clinical samples with even a very low risk of damage. "It's a rare and precious donated sample, you don't want to have a chance of damage or error," Deisseroth said. "Now the risk issue is addressed, and on top of that you can get the data very rapidly."
Fast CLARITY imaging in color
The second advance had to do this rapidity of data collection. In studying any cells, scientists often make use of probes that will go into the cell or tissue, latch onto a particular molecule, then glow green, blue, yellow or other colors in response to particular wavelengths of light. This is what produces the colorful cellular images that are so common in biology research. Using CLARITY, these colorful structures become visible throughout the entire brain, since no fat remains to block the light.
But here's the hitch. Those probes stop working, or get bleached, after they've been exposed to too much light. That's fine if a scientist is just taking a picture of a small cellular structure, which takes little time. But to get a high-resolution image of an entire brain, the whole tissue is bathed in light throughout the time it takes to image it point by point. This approach bleaches out the probes before the entire brain can be imaged at high resolution.
The second advance of the new paper addresses this issue, making it easier to image the entire brain without bleaching the probes. "We can now scan an entire plane at one time instead of a point," Deisseroth said. "That buys you a couple orders of magnitude of time, and also efficiently delivers light only to where the imaging is happening." The technique is called light sheet microscopy and has been around for a while, but previously didn't have high enough resolution to see the fine details of cellular structures. "We advanced traditional light sheet microscopy for CLARITY, and can now see fine wiring structures deep within an intact adult brain," Deisseroth said. His lab built their own microscope, but the procedures are described in the paper, and the key components are commercially available. Additionally, Deisseroth's lab provides free training courses in CLARITY, modeled after his optogenetics courses, to help disseminate the techniques.
Brain imaging to help soldiers
The BRAIN Initiative is being funded through several government agencies including the Defense Advanced Research Projects Agency (DARPA), which funded Deisseroth's work through its new Neuro-FAST program. Deisseroth said that like the National Institute of Mental Health (NIMH, another major funder of the new paper), DARPA "is interested in deepening our understanding of brain circuits in intact and injured brains to inform the development of better therapies." The new methods Deisseroth and his team developed will accelerate both human- and animal-model CLARITY; as CLARITY becomes more widely used, it will continue to help reveal how those inner circuits are structured in normal and diseased brains, and perhaps point to possible therapies.
###
Other arms of the BRAIN Initiative are funded through the National Science Foundation (NSF) and the National Institutes of Health (NIH). A working group for the NIH arm was co-led by William Newsome, professor of neurobiology and director of the Stanford Neurosciences Institute, and also included Deisseroth and Mark Schnitzer, associate professor of biology and of applied physics. That group recently recommended a $4.5 billion investment in the BRAIN Initiative over the next 12 years, which NIH Director Francis Collins approved earlier this month."
In addition to funding by DARPA and NIMH, the work was funded by the NSF, the National Institute on Drug Abuse, the Simons Foundation and the Wiegers Family Fund.
For more information on the brain, mental health, and social work topics please visit Professional Counselor Continuing Education
April 02, 2014
Autism Spectrum Disorder: Uncovering Clues to a Complicated Condition
Autism Spectrum Disorder
Uncovering Clues to a Complicated Condition
Autism is a complex brain disorder that first appears during early childhood. It affects how a person behaves and interacts with others. People with autism might not look you in the eye when talking. They may spend a lot of time lining up toys or other objects. Or they may say the same sentence over and over.
The disorder is so variable—affecting each person in very different ways—that it can be difficult to diagnose and treat. This variability is why autism is called a “spectrum” disorder. It spans the spectrum from mild to severe and includes a wide range of symptoms.
NIH-funded scientists have been working to uncover the secrets of autism. They’ve identified genes that may boost the risk for autism. They’ve developed therapies that can help many of those affected. And they’ve found that starting treatment as early as possible can lead to better outcomes. Still, there’s much more we need to learn about this complicated condition.
About 1 in 88 children may have autism spectrum disorder, according to the U.S. Centers for Disease Control and Prevention. The number of affected children has been growing in recent years. Many researchers believe this increase is due to better diagnosis and awareness. Others suspect that yet-unknown factors may be partly to blame.
Although the exact causes of autism are unclear, research suggests that both genes and the environment play important roles. Autism affects a child’s development in different ways, and so it’s known as a developmental disorder.
Parents are often the first to suspect that something may not be quite right with their child’s development. They may notice their baby doesn’t make eye contact, becomes overly focused on certain objects or isn’t “babbling” like other children the same age.
“A parent may first have concerns when a child is under 2 years of age,” says Dr. Connie Kasari, a child development expert at the University of California, Los Angeles. “A more certain diagnosis can usually be made by age 2, but some cases might not be clear until much later.”
There are no direct tests, like blood tests or brain scans, that can identify autism. Instead, the condition is diagnosed by looking at a child’s behaviors and development.
“All affected children have some sort of social impairment, but symptoms vary along a continuum,” Kasari says. “Impairment can range from kids who are in their ‘own world’ and seemingly unaware of others to high-functioning individuals who are just awkward and seem to miss the point of social interactions.”
In May 2013, the American Psychiatric Association updated an important book that’s used to diagnose and classify mental disorders. The DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th edition) includes an updated definition for autism spectrum disorder. The condition is now identified by looking for 2 broad categories of symptoms: problems with social communication and the presence of “stereotyped” behaviors, such as walking in certain patterns or insisting on specific or unusual routines. To be diagnosed with autism, these symptoms must arise during early childhood, even if they’re not noticed until later, when social demands increase.
“The new DSM-5 definition moves all the disorders into a single spectrum, rather than the 4 separate autistic disorders described in the past,” says NIH pediatrician and neuroscientist Dr. Susan Swedo. She chaired the expert panel that updated the DSM-5 definition of autism spectrum disorders. “The new criteria are also more inclusive of minorities, adolescents and young adults with autism than the previous edition, which focused more on boys ages 4 to 9.”
Getting diagnosed as early as possible is crucial. “Autism is treatable even though it’s not curable,” says Dr. David Mandell, an expert in autism and health services at the University of Pennsylvania. “If we intervene early enough with appropriate and intensive care, we can reduce a lot of impairments for many kids who have autism.”
Research has shown that therapies focusing on behavior and communication can be helpful. Some drugs can also reduce certain related symptoms, but no medications have been approved by the U.S. Food and Drug Administration specifically for treating the main symptoms of autism.
“Because autism is such a complicated disorder, no one therapy fits everyone,” Kasari explains.
Kasari and her colleagues developed and tested several treatments that focus on improving social skills and communication. In one study, preschoolers with autism received intense training in basic skills such as playing and sharing attention. Five years later, these children tended to have stronger vocabularies and better communication skills than children who received standard therapy.
“We’ve found that if we can improve these basic skills, we can also improve language learning for these kids,” Kasari says. “We’re now studying 2 potential therapies in at-risk babies, ages 12- to 21-months old, to see if we can push language development along faster for the children.”
Scientists are also looking for ways to predict likely outcomes for children with autism. One NIH-funded team found that the brain waves of some 2-year-olds with autism can have a distinctive pattern when they listen to familiar words. The children with more severe social symptoms didn’t have a typical focused response in the brain region that processes language. Follow-up studies showed that these brain responses predicted the children’s developmental abilities 2 and 4 years later.
“In the future, we’d like to be able to assess a child based on brain function or their genetic profile and then identify the intervention that might be best for that particular kid,” Mandell says.
A growing number of studies are looking at autism in older age groups. “While we think about autism as a disorder of childhood, it actually continues through adolescence and into adulthood,” Mandell says. “Some adults with autism have been misdiagnosed, and they can find themselves being treated for other conditions. We’d like to develop better screening tools and ultimately provide these adults with skills and supports to help them become happy and productive citizens.”
While research is ongoing, it’s clear that early diagnosis and treatment can improve outcomes for those with autism. If you’re concerned about your child’s social communication and behaviors, don’t wait. Talk with your child’s doctor. You may be referred to a specialist who can do a thorough evaluation. The earlier autism is diagnosed, the sooner specific therapy can begin Social Worker Continuing Education
March 24, 2014
Brain Region Singled Out for Social Memory, Possible Therapeutic Target for Select Brain Disorders
Researchers have found in mice that a formerly obscure region of the hippocampus called CA2 is important for social memory, the ability of an animal to recognize another of the same species. Identifying the role of this region could be useful in understanding and treating disorders characterized by altered social behaviors such as schizophrenia, bipolar disorder, and autism. Funded in part by the National Institute of Mental Health (NIMH), the study was published last month online in Nature.
Background
The hippocampus is essential for learning and memory—specifically the storage of knowledge of who, what, where, and when. Clues about the hippocampus’s roles emerged from the famous case of patient HM (Henry Molaison), who had most of his hippocampus removed by surgeons in 1953 to cure his epilepsy. HM became unable to form new memories of people he subsequently worked with for years.
Most previous studies of how memory is harnessed have focused on the trisynaptic pathway. In this neural circuit, information that is obtained from the entorhinal cortex—the main interface between the hippocampus and the neocortex or the outermostpart of the brain involved in higher functions such as thought or action—proceeds to the dentate gyrus, the front gate of the hippocampus. Granule neurons from the dentate gyrus then shuttle the information to interneurons and pyramidal cells of the CA3 region of the hippocampus, which then sends the information to the CA1 region, the main source of hippocampal output. Absent from this circuit is the CA2 subfield.
“Although the CA2 subregion was discovered over 75 years ago, it has received very little attention,” said Steven A. Siegelbaum, Ph.D., lead author of the study.
He ascribes two reasons for the inattention: size and location. CA2 has 10 percent the number of neurons of CA1 or CA3, raising questions about its importance. The region is also squeezed between CA1 and CA3, making it difficult to study with traditional approaches of physical or chemical lesions, which lack the precision to selectively target CA2.
To circumvent these problems, Siegelbaum, a neuroscience professor at Columbia University and a Howard Hughes Medical Institute Investigator, and Frederick L. Hitti, an M.D.-Ph.D. student, generated a special transgenic mouse in which the CA2 neurons could be selectively inhibited in adult animals. Once these neurons were inactivated, the mice underwent a series of behavioral tests.
Results of the Study
Normally when a mouse encounters another mouse it does not know, it gives it a “sniff test” and is more interested in this new mouse versus a familiar acquaintance. The CA2-inactive mouse, however, shows no recognition of mice it has seen before and ends up sniffing indiscriminately familiar and novel mice. The mice showed no loss in the ability to discriminate social or non-social odors, such as food buried deeply in its litterbox. Although a pronounced loss of social memory is seen in the CA2-inactive mice, the mice did not experience changes in other hippocampal-specific behaviors such as spatial and contextual memory, and could still distinguish between novel and familiar inanimate objects.
Significance
“Because several neuropsychiatric disorders are associated with altered social behaviors, our findings raise the possibility that CA2 dysfunction may contribute to these behavioral changes,” said Siegelbaum.
Individuals with schizophrenia and bipolar disorder have lowered numbers of CA2 inhibitory neurons. Similarly, individuals with autism have altered signaling of vasopressin, a social behavior hormone that interacts with a specific class of receptors found predominantly in this region. However, the CA2-inactive mice did not display classic symptoms of autism as they had normal levels of sociability, providing evidence that sociability and social memory involve different brain functions. Techniques such as the one detailed here are examples of research tools that the NIH Brain Research through Advancing Innovative Neurotechnologies (BRAIN ) Initiative hopes to build upon to further our understanding of the human brain.
What’s Next
Siegelbaum’s group hopes to use the same genetic technology to examine whether there are changes in CA2 function in mouse models of psychiatric disorders such as autism and schizophrenia. If so, they plan to screen for drugs that restore normal CA2 function and ask whether this drug treatment helps reverse any behavioral changes seen in the mice. Such research offers the possibility of finding new drug targets and approaches for treating the behavioral changes associated with these disorders Alcoholism and Drug Abuse Counselors Continuing Education
Reference
Hitti FL, Siegelbaum SA. The Hippocampal CA2 Region is Essential for Social Memory. Nature , published online February 23, 2014.
Grant 5F30MH098633-02
March 12, 2014
Researchers pinpoint brain region essential for social memory
Potential target for treating autism, schizophrenia, and other brain disorders
NEW YORK, NY (February 23, 2014) — Columbia University Medical Center (CUMC) researchers have determined that a small region of the hippocampus known as CA2 is essential for social memory, the ability of an animal to recognize another of the same species. A better grasp of the function of CA2 could prove useful in understanding and treating disorders characterized by altered social behaviors, such as autism, schizophrenia, and bipolar disorder. The findings, made in mice, were published today in the online edition of Nature.
Scientists have long understood that the hippocampus—a pair of seahorse-shaped structures in the brain's temporal lobes—plays a critical role in our ability to remember the who, what, where, and when of our daily lives. Recent studies have shown that different subregions of the hippocampus have different functions. For instance, the dentate gyrus is critical for distinguishing between similar environments, while CA3 enables us to recall a memory from partial cues (e.g., Proust's famous madeleine). The CA1 region is critical for all forms of memory.
"However, the role of CA2, a relatively small region of the hippocampus sandwiched between CA3 and CA1, has remained largely unknown," said senior author Steven A. Siegelbaum, PhD, professor of neuroscience and pharmacology, chair of the Department of Neuroscience, a member of the Mortimer B. Zuckerman Mind Brain Behavior Institute and Kavli Institute for Brain Science, and a Howard Hughes Medical Institute Investigator. A few studies have suggested that CA2 might be involved in social memory, as this region has a high level of expression of a receptor for vasopressin, a hormone linked to sexual motivation, bonding, and other social behaviors.
To learn more about this part of the hippocampus, the researchers created a transgenic mouse in which CA2 neurons could be selectively inhibited in adult animals. Once the neurons were inhibited, the mice were given a series of behavioral tests. "The mice looked quite normal until we looked at social memory," said first author Frederick L. Hitti, an MD-PhD student in Dr. Siegelbaum's laboratory, who developed the transgenic mouse. "Normally, mice are naturally curious about a mouse they've never met; they spend more time investigating an unfamiliar mouse than a familiar one. In our experiment, however, mice with an inactivated CA2 region showed no preference for a novel mouse versus a previously encountered mouse, indicating a lack of social memory."
In two separate novel-object recognition tests, the CA2-deficient mice showed a normal preference for an object they had not previously encountered, showing that the mice did not have a global lack of interest in novelty. In another experiment, the researchers tested whether the animals' inability to form social memories might have to do with deficits in olfaction (sense of smell), which is crucial for normal social interaction. However, the mice showed no loss in ability to discriminate social or non-social odors.
In humans, the importance of the hippocampus for social memory was famously illustrated by the case of Henry Molaison, who had much of his hippocampus removed by surgeons in 1953 in an attempt to cure severe epilepsy. Molaison (often referred to as HM in the scientific literature) was subsequently unable to form new memories of people. Scientists have observed that lesions limited to the hippocampus also impair social memory in both rodents and humans.
"Because several neuropsychiatric disorders are associated with altered social behaviors, our findings raise the possibility that CA2 dysfunction may contribute to these behavioral changes," said Dr. Siegelbaum. This possibility is supported by findings of a decreased number of CA2 inhibitory neurons in individuals with schizophrenia and bipolar disorder and altered vasopressin signaling in autism. Thus, CA2 may provide a new target for therapeutic approaches to the treatment of social disorders.
The paper is titled, "The hippocampal CA2 region is essential for social memory."
###
The study was supported by a Ruth L. Kirschstein F30 National Research Service Award from the National Institute of Mental Health and the Howard Hughes Medical Institute.
The authors declare no financial or other conflicts of interests.
The Mortimer B. Zuckerman Mind Brain Behavior Institute
Columbia University's Mortimer B. Zuckerman Mind Brain Behavior Institute is an interdisciplinary hub for scholars across the university, created on a scope and scale to explore the human brain and behavior at levels of inquiry from cells to society. The institute's leadership, which includes two Nobel Prize-winning neuroscientists, and many of its principal investigators will be based at the 450,000-square-foot Jerome L. Greene Science Center, now rising on the university's new Manhattanville campus. In combining Columbia's preeminence in neuroscience with its strengths in the biological and physical sciences, social sciences, arts, and humanities, the institute provides a common intellectual forum for research communities from Columbia University Medical Center, the Faculty of Arts and Sciences, the School of Engineering and Applied Science, and professional schools on both the Morningside Heights and Washington Heights campuses. Their collective mission is to further our understanding of the human condition and to find cures for disease.
Columbia University Medical Center provides international leadership in basic, preclinical, and clinical research; medical and health sciences education; and patient care. The medical center trains future leaders and includes the dedicated work of many physicians, scientists, public health professionals, dentists, and nurses at the College of Physicians and Surgeons, the Mailman School of Public Health, the College of Dental Medicine, the School of Nursing, the biomedical departments of the Graduate School of Arts and Sciences, and allied research centers and institutions. Columbia University Medical Center is home to the largest medical research enterprise in New York City and State and one of the largest faculty medical practices in the Northeast. For more information, visit cumc.columbia.edu or columbiadoctors.org.
For more information on related mental health, nursing and social work topics, visit Continuing Education for Social Workers
February 12, 2014
New evidence that chronic stress predisposes brain to mental illness
By Robert Sanders, Media Relations | February 11, 2014
BERKELEY —
University of California, Berkeley, researchers have shown that chronic stress generates long-term changes in the brain that may explain why people suffering chronic stress are prone to mental problems such as anxiety and mood disorders later in life.
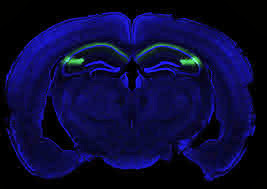
myelin stained blue
Myelin is stained blue in this cross section of a rat hippocampus. Myelin, which speeds electrical signals flowing through axons, is produced by oligodendrocytes, which increase in number as a result of chronic stress. New oligodendrocytes are shown in yellow. Image by Aaron Friedman and Daniela Kaufer.
Their findings could lead to new therapies to reduce the risk of developing mental illness after stressful events.
Doctors know that people with stress-related illnesses, such as post-traumatic stress disorder (PTSD), have abnormalities in the brain, including differences in the amount of gray matter versus white matter. Gray matter consists mostly of cells – neurons, which store and process information, and support cells called glia – while white matter is comprised of axons, which create a network of fibers that interconnect neurons. White matter gets its name from the white, fatty myelin sheath that surrounds the axons and speeds the flow of electrical signals from cell to cell.
How chronic stress creates these long-lasting changes in brain structure is a mystery that researchers are only now beginning to unravel.
In a series of experiments, Daniela Kaufer, UC Berkeley associate professor of integrative biology, and her colleagues, including graduate students Sundari Chetty and Aaron Freidman, discovered that chronic stress generates more myelin-producing cells and fewer neurons than normal. This results in an excess of myelin – and thus, white matter – in some areas of the brain, which disrupts the delicate balance and timing of communication within the brain.
“We studied only one part of the brain, the hippocampus, but our findings could provide insight into how white matter is changing in conditions such as schizophrenia, autism, depression, suicide, ADHD and PTSD,” she said.
The hippocampus regulates memory and emotions, and plays a role in various emotional disorders.
Kaufer and her colleagues published their findings in the Feb. 11 issue of the journal Molecular Psychiatry.
Does stress affect brain connectivity?
Kaufer’s findings suggest a mechanism that may explain some changes in brain connectivity in people with PTSD, for example. One can imagine, she said, that PTSD patients could develop a stronger connectivity between the hippocampus and the amygdala – the seat of the brain’s fight or flight response – and lower than normal connectivity between the hippocampus and prefrontal cortex, which moderates our responses.
“You can imagine that if your amygdala and hippocampus are better connected, that could mean that your fear responses are much quicker, which is something you see in stress survivors,” she said. “On the other hand, if your connections are not so good to the prefrontal cortex, your ability to shut down responses is impaired. So, when you are in a stressful situation, the inhibitory pathways from the prefrontal cortex telling you not to get stressed don’t work as well as the amygdala shouting to the hippocampus, ‘This is terrible!’ You have a much bigger response than you should.”
white matter fibers in human brain
White matter fiber architecture of the brain. Human Connectome Project.
She is involved in a study to test this hypothesis in PTSD patients, and continues to study brain changes in rodents subjected to chronic stress or to adverse environments in early life.
Stress tweaks stem cells
Kaufer’s lab, which conducts research on the molecular and cellular effects of acute and chronic stress, focused in this study on neural stem cells in the hippocampus of the brains of adult rats. These stem cells were previously thought to mature only into neurons or a type of glial cell called an astrocyte. The researchers found, however, that chronic stress also made stem cells in the hippocampus mature into another type of glial cell called an oligodendrocyte, which produces the myelin that sheaths nerve cells.
The finding, which they demonstrated in rats and cultured rat brain cells, suggests a key role for oligodendrocytes in long-term and perhaps permanent changes in the brain that could set the stage for later mental problems. Oligodendrocytes also help form synapses – sites where one cell talks to another – and help control the growth pathway of axons, which make those synapse connections.
The fact that chronic stress also decreases the number of stem cells that mature into neurons could provide an explanation for how chronic stress also affects learning and memory, she said.
Kaufer is now conducting experiments to determine how stress in infancy affects the brain’s white matter, and whether chronic early-life stress decreases resilience later in life. She also is looking at the effects of therapies, ranging from exercise to antidepressant drugs, that reduce the impact of stress and stress hormones.
Kaufer’s coauthors include Chetty, formerly from UC Berkeley’s Helen Wills Neuroscience Institute and now at Harvard University; Friedman and K. Taravosh-Lahn at UC Berkeley’s Department of Integrative Biology; additional colleagues from UC Berkeley and others from Stanford University and UC Davis.
The work was supported by a BRAINS (Biobehavioral Research Awards for Innovative New Scientists) award from the National Institute of Mental Health of the National Institutes of Health (R01 MH087495), a Berkeley Stem Cell Center Seed Grant, the Hellman Family Foundation and the National Alliance for Research on Schizophrenia and Depression.
RELATED INFORMATION
•Stress and glucocorticoids promote oligodendrogenesis in the adult hippocampus (2/11/14 Molecular Psychiatry)
•Daniela Kaufer’s web site
•Researchers find out why some stress is good for you (4/16/13 press release)
For more information on this and other mental health topics, please visit Counselor CEUs
Labels:
brain,
counselor ceus,
hippocampus,
mental illness,
neuroscience,
psychiatry,
stress
January 15, 2014
SHY hypothesis explains that sleep is the price we pay for learning
MADISON — Why do animals ranging from fruit flies to humans all need to sleep? After all, sleep disconnects them from their environment, puts them at risk and keeps them from seeking food or mates for large parts of the day.
Two leading sleep scientists from the University of Wisconsin School of Medicine and Public Health say that their synaptic homeostasis hypothesis of sleep or "SHY" challenges the theory that sleep strengthens brain connections. The SHY hypothesis, which takes into account years of evidence from human and animal studies, says that sleep is important because it weakens the connections among brain cells to save energy, avoid cellular stress, and maintain the ability of neurons to respond selectively to stimuli.
"Sleep is the price the brain must pay for learning and memory," says Dr. Giulio Tononi, of the UW Center for Sleep and Consciousness. "During wake, learning strengthens the synaptic connections throughout the brain, increasing the need for energy and saturating the brain with new information. Sleep allows the brain to reset, helping integrate, newly learned material with consolidated memories, so the brain can begin anew the next day. "
Tononi and his co-author Dr. Chiara Cirelli, both professors of psychiatry, explain their hypothesis in a review article in today's issue of the journal Neuron. Their laboratory studies sleep and consciousness in animals ranging from fruit flies to humans; SHY takes into account evidence from molecular, electrophysiological and behavioral studies, as well as from computer simulations. "Synaptic homeostasis" refers to the brain's ability to maintain a balance in the strength of connections within its nerve cells.
Why would the brain need to reset? Suppose someone spent the waking hours learning a new skill, such as riding a bike. The circuits involved in learning would be greatly strengthened, but the next day the brain will need to pay attention to learning a new task. Thus, those bike-riding circuits would need to be damped down so they don't interfere with the new day's learning.
"Sleep helps the brain renormalize synaptic strength based on a comprehensive sampling of its overall knowledge of the environment," Tononi says, "rather than being biased by the particular inputs of a particular waking day."
The reason we don't also forget how to ride a bike after a night's sleep is because those active circuits are damped down less than those that weren't actively involved in learning. Indeed, there is evidence that sleep enhances important features of memory, including acquisition, consolidation, gist extraction, integration and "smart forgetting," which allows the brain to rid itself of the inevitable accumulation of unimportant details. However, one common belief is that sleep helps memory by further strengthening the neural circuits during learning while awake. But Tononi and Cirelli believe that consolidation and integration of memories, as well as the restoration of the ability to learn, all come from the ability of sleep to decrease synaptic strength and enhance signal-to-noise ratios.
While the review finds testable evidence for the SHY hypothesis, it also points to open issues. One question is whether the brain could achieve synaptic homeostasis during wake, by having only some circuits engaged, and the rest off-line and thus resetting themselves. Other areas for future research include the specific function of REM sleep (when most dreaming occurs) and the possibly crucial role of sleep during development, a time of intense learning and massive remodeling of brain Counselor CEUs
Labels:
brain,
counselor ceus,
forgetting,
hypothesis,
psychiatry,
shy,
sleep
December 18, 2013
Heavy marijuana users have abnormal brain structure and poor memory
Drug abuse appears to foster brain changes that resemble schizophrenia
CHICAGO --- Teens who were heavy marijuana users -- smoking it daily for about three years -- had abnormal changes in their brain structures related to working memory and performed poorly on memory tasks, reports a new Northwestern Medicine® study.
A poor working memory predicts poor academic performance and everyday functioning.
The brain abnormalities and memory problems were observed during the individuals' early twenties, two years after they stopped smoking marijuana, which could indicate the long-term effects of chronic use. Memory-related structures in their brains appeared to shrink and collapse inward, possibly reflecting a decrease in neurons.
The study also shows the marijuana-related brain abnormalities are correlated with a poor working memory performance and look similar to schizophrenia-related brain abnormalities. Over the past decade, Northwestern scientists, along with scientists at other institutions, have shown that changes in brain structure may lead to changes in the way the brain functions.
This is the first study to target key brain regions in the deep subcortical gray matter of chronic marijuana users with structural MRI and to correlate abnormalities in these regions with an impaired working memory. Working memory is the ability to remember and process information in the moment and -- if needed -- transfer it to long-term memory. Previous studies have evaluated the effects of marijuana on the cortex, and few have directly compared chronic marijuana use in otherwise healthy individuals and individuals with schizophrenia.
The younger the individuals were when they started chronically using marijuana, the more abnormally their brain regions were shaped, the study reports. The findings suggest that these regions related to memory may be more susceptible to the effects of the drug if abuse starts at an earlier age.
"The study links the chronic use of marijuana to these concerning brain abnormalities that appear to last for at least a few years after people stop using it," said lead study author Matthew Smith, an assistant research professor in psychiatry and behavioral sciences at Northwestern University Feinberg School of Medicine. "With the movement to decriminalize marijuana, we need more research to understand its effect on the brain." Alcoholism and Drug Abuse Counselors Continuing Education
The paper will be published Dec. 16 in the journal Schizophrenia Bulletin.
In the U.S., marijuana is the most commonly used illicit drug and young adults have the highest -- and growing -- prevalence of use. Decriminalization of the drug may lead to greater use.
Because the study results examined one point in time, a longitudinal study is needed to definitively show if marijuana is responsible for the brain changes and memory impairment. It is possible that the abnormal brain structures reveal a pre-existing vulnerability to marijuana abuse. But evidence that the younger a subject started using the drug the greater his brain abnormality indicates marijuana may be the cause, Smith said.
The groups in the study started using marijuana daily between 16 to 17 years of age for about three years. At the time of the study, they had been marijuana free for about two years. A total of 97 subjects participated, including matched groups of healthy controls, subjects with a marijuana use disorder, schizophrenia subjects with no history of substance use disorders, and schizophrenia subjects with a marijuana use disorder. The subjects who used marijuana did not abuse any other drugs.
Few studies have examined marijuana's effect on the deep regions in the brain -- the 'subcortical gray matter' below the noodle-shaped cortex. The study also is unique in that it looked at the shapes of the striatum, globus pallidus and thalamus, structures in the subcortex that are critical for motivation and working memory.
The Marijuana and Schizophrenia Connection
Chronic use of marijuana may contribute to changes in brain structure that are associated with having schizophrenia, the Northwestern research shows. Of the 15 marijuana smokers who had schizophrenia in the study, 90 percent started heavily using the drug before they developed the mental disorder. Marijuana abuse has been linked to developing schizophrenia in prior research.
"The abuse of popular street drugs, such as marijuana, may have dangerous implications for young people who are developing or have developed mental disorders," said co-senior study author John Csernansky, M.D., chair of psychiatry and behavioral sciences at Northwestern University Feinberg School of Medicine and Northwestern Memorial Hospital. "This paper is among the first to reveal that the use of marijuana may contribute to the changes in brain structure that have been associated with having schizophrenia."
Chronic marijuana use could augment the underlying disease process associated with schizophrenia, Smith noted. "If someone has a family history of schizophrenia, they are increasing their risk of developing schizophrenia if they abuse marijuana," he said.
While chronic marijuana smokers and chronic marijuana smokers with schizophrenia both had brain changes related to the drug, subjects with the mental disorder had greater deterioration in the thalamus. That structure is the communication hub of the brain and is critical for learning, memory and communications between brain regions. The brain regions examined in this study also affect motivation, which is already notably impaired in people with schizophrenia.
"A tremendous amount of addiction research has focused on brain regions traditionally connected with reward/aversion function, and thus motivation," noted co-senior study author Hans Breiter, M.D., professor of psychiatry and behavioral sciences and director of the Warren Wright Adolescent Center at Feinberg and Northwestern Memorial. "This study very nicely extends the set of regions of concern to include those involved with working memory and higher level cognitive functions necessary for how well you organize your life and can work in society."
"If you have schizophrenia and you frequently smoke marijuana, you may be at an increased risk for poor working memory, which predicts your everyday functioning," Smith said.
###
The research was supported by grants R01 MH056584 and P50 MH071616 from the National Institute of Mental Health and grants P20 DA026002 and RO1 DA027804 from National Institute of Drug Abuse, all of the National Institutes of Health.
December 10, 2013
Gene found to be crucial for formation of certain brain circuitry
Identified using new technique that can speed identification of genes, drug candidates
Using a powerful gene-hunting technique for the first time in mammalian brain cells, researchers at Johns Hopkins report they have identified a gene involved in building the circuitry that relays signals through the brain. The gene is a likely player in the aging process in the brain, the researchers say. Additionally, in demonstrating the usefulness of the new method, the discovery paves the way for faster progress toward identifying genes involved in complex mental illnesses such as autism and schizophrenia — as well as potential drugs for such conditions. A summary of the study appears in the Dec. 12 issue of Cell Reports.
"We have been looking for a way to sift through large numbers of genes at the same time to see whether they affect processes we're interested in," says Richard Huganir, Ph.D., director of the Johns Hopkins University Solomon H. Snyder Department of Neuroscience and a Howard Hughes Medical Institute investigator, who led the study. "By adapting an automated process to neurons, we were able to go through 800 genes to find one needed for forming synapses — connections — among those cells."
Although automated gene-sifting techniques have been used in other areas of biology, Huganir notes, many neuroscience studies instead build on existing knowledge to form a hypothesis about an individual gene's role in the brain. Traditionally, researchers then disable or "knock out" the gene in lab-grown cells or animals to test their hypothesis, a time-consuming and laborious process.
In this study, Huganir's group worked to test many genes all at once using plastic plates with dozens of small wells. A robot was used to add precise allotments of cells and nutrients to each well, along with molecules designed to knock out one of the cells' genes — a different one for each well.
"The big challenge was getting the neurons, which are very sensitive, to function under these automated conditions," says Kamal Sharma, Ph.D., a research associate in Huganir's group. The team used a trial-and-error approach, adjusting how often the nutrient solution was changed and adding a washing step, and eventually coaxed the cells to thrive in the wells. In addition, Sharma says, they fine-tuned an automated microscope used to take pictures of the circuitry that had formed in the wells and calculated the numbers of synapses formed among the cells.
The team screened 800 genes in this way and found big differences in the well of cells with a gene called LRP6 knocked out. LRP6 had previously been identified as a player in a biochemical chain of events known as the Wnt pathway, which controls a range of processes in the brain. Interestingly, Sharma says, the team found that LRP6 was only found on a specific kind of synapse known as an excitatory synapse, suggesting that it enables the Wnt pathway to tailor its effects to just one synapse type.
"Changes in excitatory synapses are associated with aging, and changes in the Wnt pathway in later life may accelerate aging in general. However, we do not know what changes take place in the synaptic landscape of the aging brain. Our findings raise intriguing questions: Is the Wnt pathway changing that landscape, and if so, how?" says Sharma. "We're interested in learning more about what other proteins LRP6 interacts with, as well as how it acts in different types of brain cells at different developmental stages of circuit development and refinement."
Another likely outcome of the study is wider use of the gene-sifting technique, he says, to explore the genetics of complex mental illnesses. The automated method could also be used to easily test the effects on brain cells of a range of molecules and see which might be drug candidates Continuing Education for Social Workers
###
Other authors on the paper are Se-Young Choi, now of Seoul National University School of Dentistry; Yong Zhang, Shunyou Long and Min Li of Johns Hopkins University School of Medicine; and Thomas J.F. Nieland, now of the Broad Institute of Harvard and MIT. This work was supported by grants from the Howard Hughes Medical Institute and the National Institute of Mental Health (grant numbers P50MH084020 and 5U54MH084691).
Related stories:
Gene Found to Foster Synapse Formation in the Brain http://www.hopkinsmedicine.org/news/media/releases/gene_found_to_foster_synapse_formation_in_the_brain
Study Refutes Accepted Model of Memory Formation http://www.hopkinsmedicine.org/news/media/releases/study_refutes_accepted_model_of_memory_formation____
Newly Discovered "Switch" Plays Dual Role in Memory Formation http://m.hopkinsmedicine.org/news/media/releases/newly_discovered_switch_plays_dual_role_in_memory_formation
December 03, 2013
Brain connectivity study reveals striking differences between men and women
Penn Medicine brain imaging study helps explain different cognitive strengths in men and women
PHILADELPHIA—A new brain connectivity study from Penn Medicine published today in the Proceedings of National Academy of Sciences found striking differences in the neural wiring of men and women that's lending credence to some commonly-held beliefs about their behavior.
In one of the largest studies looking at the "connectomes" of the sexes, Ragini Verma, PhD, an associate professor in the department of Radiology at the Perelman School of Medicine at the University of Pennsylvania, and colleagues found greater neural connectivity from front to back and within one hemisphere in males, suggesting their brains are structured to facilitate connectivity between perception and coordinated action. In contrast, in females, the wiring goes between the left and right hemispheres, suggesting that they facilitate communication between the analytical and intuition.
"These maps show us a stark difference--and complementarity--in the architecture of the human brain that helps provide a potential neural basis as to why men excel at certain tasks, and women at others," said Verma.
For instance, on average, men are more likely better at learning and performing a single task at hand, like cycling or navigating directions, whereas women have superior memory and social cognition skills, making them more equipped for multitasking and creating solutions that work for a group. They have a mentalistic approach, so to speak.
Past studies have shown sex differences in the brain, but the neural wiring connecting regions across the whole brain that have been tied to such cognitive skills has never been fully shown in a large population.
In the study, Verma and colleagues, including co-authors Ruben C. Gur, PhD, a professor of psychology in the department of Psychiatry, and Raquel E. Gur, MD, PhD, professor of Psychiatry, Neurology and Radiology, investigated the gender-specific differences in brain connectivity during the course of development in 949 individuals (521 females and 428 males) aged 8 to 22 years using diffusion tensor imaging (DTI). DTI is water-based imaging technique that can trace and highlight the fiber pathways connecting the different regions of the brain, laying the foundation for a structural connectome or network of the whole brain.
This sample of youths was studied as part of the Philadelphia Neurodevelopmental Cohort, a National Institute of Mental Health-funded collaboration between the University of Pennsylvania Brain Behavior Laboratory and the Center for Applied Genomics at the Children's Hospital of Philadelphia.
The brain is a roadmap of neural pathways linking many networks that help us process information and react accordingly, with behavior controlled by several of these sub-networks working in conjunction.
In the study, the researchers found that females displayed greater connectivity in the supratentorial region, which contains the cerebrum, the largest part of the brain, between the left and right hemispheres. Males, on the other hand, displayed greater connectivity within each hemisphere.
By contrast, the opposite prevailed in the cerebellum, the part of the brain that plays a major role in motor control, where males displayed greater inter-hemispheric connectivity and females displayed greater intra-hemispheric connectivity.
These connections likely give men an efficient system for coordinated action, where the cerebellum, which involves perception, and the front of the brain, which involves action, are bridged together, according to the authors. The female connections likely facilitate integration of the analytic and sequential processing modes of the left hemisphere with the spatial, intuitive information processing modes of the right side.
The authors observed only a few gender differences in the connectivity in children younger than 13 years, but the differences were more pronounced in adolescents aged 14 to 17 years and young adults older than 17.
The findings were also consistent with a Penn behavior study, of which this imaging study was a subset of, that demonstrated pronounced sexual differences. Females outperformed males on attention, word and face memory, and social cognition tests. Males performed better on spatial processing and sensorimotor speed. Those differences were most pronounced in the 12 to 14 age range.
"It's quite striking how complementary the brains of women and men really are," said Dr. Ruben Gur. "Detailed connectome maps of the brain will not only help us better understand the differences between how men and women think, but it will also give us more insight into the roots of neuropsychiatric disorders, which are often sex related."
Next steps are to quantify how an individual's neural connections are different from the population; identify which neural connections are gender specific and common in both; and to see if findings from functional magnetic resonance imaging (fMRI) studies fall in line with the connectome data Professional Counselor Continuing Education
###
Co-authors of the study include Madhura Ingalhalikar, Alex Smith, Drew Parker, Theodore D. Satterthwaite, Mark A. Elliott, Kosha Ruparel, and Hakon Hakonarson of the Section of Biomedical Image Analysis and the Center for Biomedical Image Computing and Analytics.
This study was funded by in part by the National Institutes of Mental Health: MH089983, MH089924, MH079938, and MH092862.
November 10, 2013
OHSU Vollum Institute research gives new insight into how antidepressants work in the brain
Vollum Institute scientist publishes two papers on neurotransmission in today’s edition of Nature
Research from Oregon Health & Science University's Vollum Institute, published in the current issue of Nature, is giving scientists a never-before-seen view of how nerve cells communicate with each other. That new view can give scientists a better understanding of how antidepressants work in the human brain — and could lead to the development of better antidepressants with few or no side effects.
The article in today’s edition of Nature came from the lab of Eric Gouaux, Ph.D., a senior scientist at OHSU's Vollum Institute and a Howard Hughes Medical Institute Investigator. The article describes research that gives a better view of the structural biology of a protein that controls communication between nerve cells. The view is obtained through special structural and biochemical methods Gouaux uses to investigate these neural proteins.
The Nature article focuses on the structure of the dopamine transporter, which helps regulate dopamine levels in the brain. Dopamine is an essential neurotransmitter for the human body's central nervous system; abnormal levels of dopamine are present in a range of neurological disorders, including Parkinson's disease, drug addiction, depression and schizophrenia. Along with dopamine, the neurotransmitters noradrenaline and serotonin are transported by related transporters, which can be studied with greater accuracy based on the dopamine transporter structure.
The Gouaux lab's more detailed view of the dopamine transporter structure better reveals how antidepressants act on the transporters and thus do their work Alcoholism and Drug Abuse Counselors Continuing Education
The more detailed view could help scientists and pharmaceutical companies develop drugs that do a much better job of targeting what they're trying to target — and not create side effects caused by a broader blast at the brain proteins.
"By learning as much as possible about the structure of the transporter and its complexes with antidepressants, we have laid the foundation for the design of new molecules with better therapeutic profiles and, hopefully, with fewer deleterious side effects," said Gouaux.
Gouaux's latest dopamine transporter research is also important because it was done using the molecule from fruit flies, a dopamine transporter that is much more similar to those in humans than the bacteria models that previous studies had used.
The dopamine transporter article was one of two articles Gouaux had published in today’s edition of Nature. The other article also dealt with a modified amino acid transporter that mimics the mammalian neurotransmitter transporter proteins targeted by antidepressants. It gives new insights into the pharmacology of four different classes of widely used antidepressants that act on certain transporter proteins, including transporters for dopamine, serotonin and noradrenaline. The second paper in part was validated by findings of the first paper — in how an antidepressant bound itself to a specific transporter.
"What we ended up finding with this research was complementary and mutually reinforcing with the other work — so that was really important," Gouaux said. "And it told us a great deal about how these transporters work and how they interact with the antidepressant molecules."
Gouaux's discoveries over the years in neurotransmission have established him as one of the top investigators in his field. His research has important implications for understanding the mechanisms of not just antidepressants, but also drugs used for the treatment of a wide range of psychiatric and neurological diseases.
Gouaux's co-authors on the dopamine transporter paper were both members of his lab; Aravind Penmatsa, Ph.D., and Kevin Wang, Ph.D.
Gouaux's co-authors on the second Nature paper were also members or former members of his lab: Hui Wang, Ph.D.; April Goehring, Ph.D.; Kevin Wang, Aravind Penmatsa and Ryan Ressler, Ph.D.
Both papers were funded by the American Heart Association, the National Institute of Mental Health, (1F32MH093120 and 5R37MH070039) and the Howard Hughes Medical Institute.
About the OHSU Vollum Institute
The Vollum Institute is a privately endowed research institute at OHSU and is dedicated to basic research that will lead to new treatments for neurological and psychiatric diseases. Vollum scientists have transformed the field of neuroscience and, in particular, have been pioneers in the study of cellular signaling, neuronal development, gene regulation and the neurobiology of disease.
About OHSU
Oregon Health & Science University is a nationally prominent research university and Oregon’s only public academic health center. It serves patients throughout the region with a Level 1 trauma center and nationally recognized Doernbecher Children’s Hospital. OHSU operates dental, medical, nursing and pharmacy schools that rank high both in research funding and in meeting the university’s social mission. OHSU’s Knight Cancer Institute helped pioneer personalized medicine through a discovery that identified how to shut down cells that enable cancer to grow without harming healthy ones. OHSU Brain Institute scientists are nationally recognized for discoveries that have led to a better understanding of Alzheimer’s disease and new treatments for Parkinson’s disease, multiple sclerosis and stroke. OHSU’s Casey Eye Institute is a global leader in ophthalmic imaging, and in clinical trials related to eye disease.
October 31, 2013
Gene found to foster synapse formation in the brain
Implications for language development, autism, epilepsy
Researchers at Johns Hopkins say they have found that a gene already implicated in human speech disorders and epilepsy is also needed for vocalizations and synapse formation in mice. The finding, they say, adds to scientific understanding of how language develops, as well as the way synapses — the connections among brain cells that enable us to think — are formed. A description of their experiments appears in Science Express on Oct. 31.
A group led by Richard Huganir, Ph.D., director of the Solomon H. Snyder Department of Neuroscience and a Howard Hughes Medical Institute investigator, set out to investigate genes involved in synapse formation. Gek-Ming Sia, Ph.D., a research associate in Huganir's laboratory, first screened hundreds of human genes for their effects on lab-grown mouse brain cells. When one gene, SRPX2, was turned up higher than normal, it caused the brain cells to erupt with new synapses, Sia found.
When Huganir's team injected fetal mice with an SRPX2-blocking compound, the mice showed fewer synapses than normal mice even as adults, the researchers found. In addition, when SRPX2-deficient mouse pups were separated from their mothers, they did not emit high-pitched distress calls as other pups do, indicating they lacked the rodent equivalent of early language ability.
Other researchers' analyses of the human genome have found that mutations in SRPX2 are associated with language disorders and epilepsy, and when Huganir's team injected the human SRPX2 with the same mutations into the fetal mice, they also had deficits in their vocalization as young pups.
Another research group at Institut de Neurobiologie de la Méditerranée in France had previously shown that SRPX2 interacts with FoxP2, a gene that has gained wide attention for its apparently crucial role in language ability. Huganir's team confirmed this, showing that FoxP2 controls how much protein the SRPX2 gene makes and may affect language in this way. "FoxP2 is famous for its role in language, but it's actually involved in other functions as well," Huganir comments. "SRPX2 appears to be more specialized to language ability." Huganir suspects that the gene may also be involved in autism, since autistic patients often have language impairments, and the condition has been linked to defects in synapse formation.
This study is only the beginning of teasing out how SRPX2 acts on the brain, Sia says. "We'd like to find out what other proteins it acts on, and how exactly it regulates synapses and enables language development."
Roger Clem of the Mount Sinai School of Medicine also participated in the study CADC I & II Continuing Education
###
This study was supported by the National Institute of Mental Health (grant number P50MH084020) and the National Institute of Neurological Disorders and Stroke (grant number NS050274).
Related stories:
Study Refutes Accepted Model of Memory Formation
Johns Hopkins Scientists Reveal Molecular Sculptor of Memories
Johns Hopkins Researchers Discover How to Erase Memory
Labels:
brain,
CADC I and II Continuing Education,
gene,
neuroscience,
synapse
October 29, 2013
Nurturing may protect kids from brain changes linked to poverty
Growing up in poverty can have long-lasting, negative consequences for a child. But for poor children raised by parents who lack nurturing skills, the effects may be particularly worrisome, according to a new study at Washington University School of Medicine in St. Louis.
Among children living in poverty, the researchers identified changes in the brain that can lead to lifelong problems like depression, learning difficulties and limitations in the ability to cope with stress. The study showed that the extent of those changes was influenced strongly by whether parents were nurturing.
The good news, according to the researchers, is that a nurturing home life may offset some of the negative changes in brain anatomy among poor children. And the findings suggest that teaching nurturing skills to parents — particularly those living in poverty — may provide a lifetime benefit for their children.
The study is published online Oct. 28 and will appear in the November issue of JAMA Pediatrics.
Using magnetic resonance imaging (MRI), the researchers found that poor children with parents who were not very nurturing were likely to have less gray and white matter in the brain. Gray matter is closely linked to intelligence, while white matter often is linked to the brain's ability to transmit signals between various cells and structures.
The MRI scans also revealed that two key brain structures were smaller in children who were living in poverty: the amygdala, a key structure in emotional health, and the hippocampus, an area of the brain that is critical to learning and memory.
"We've known for many years from behavioral studies that exposure to poverty is one of the most powerful predictors of poor developmental outcomes for children," said principal investigator Joan L. Luby, MD, a Washington University child psychiatrist at St. Louis Children's Hospital. "A growing number of neuroscience and brain-imaging studies recently have shown that poverty also has a negative effect on brain development.
"What's new is that our research shows the effects of poverty on the developing brain, particularly in the hippocampus, are strongly influenced by parenting and life stresses that the children experience."
Luby, a professor of psychiatry and director of the university's Early Emotional Development Program, is in the midst of a long-term study of childhood depression. As part of the Preschool Depression Study, she has been following 305 healthy and depressed kids since they were in preschool. As the children have grown, they also have received MRI scans that track brain development.
"We actually stumbled upon this finding," she said. "Initially, we thought we would have to control for the effects of poverty, but as we attempted to control for it, we realized that poverty was really driving some of the outcomes of interest, and that caused us to change our focus to poverty, which was not the initial aim of this study."
In the new study, Luby's team looked at scans from 145 children enrolled in the depression study. Some were depressed, others healthy, and others had been diagnosed with different psychiatric disorders such as ADHD (attention-deficit hyperactivity disorder). As she studied these children, Luby said it became clear that poverty and stressful life events, which often go hand in hand, were affecting brain development.
The researchers measured poverty using what's called an income-to-needs ratio, which takes a family's size and annual income into account. The current federal poverty level is $23,550 for a family of four.
Although the investigators found that poverty had a powerful impact on gray matter, white matter, hippocampal and amygdala volumes, they found that the main driver of changes among poor children in the volume of the hippocampus was not lack of money but the extent to which poor parents nurture their children. The hippocampus is a key brain region of interest in studying the risk for impairments.
Luby's team rated nurturing using observations made by the researchers — who were unaware of characteristics such as income level or whether a child had a psychiatric diagnosis — when the children came to the clinic for an appointment. And on one of the clinic visits, the researchers rated parental nurturing using a test of the child's impatience and of a parent's patience with that child.
AUDIO: Poverty can interfere with healthy development in children and can have long-lasting, negative consequences. Now researchers at Washington University School of Medicine in St. Louis have found that if poor...
Click here for more information.
While waiting to see a health professional, a child was given a gift-wrapped package, and that child's parent or caregiver was given paperwork to fill out. The child, meanwhile, was told that s/he could not open the package until the caregiver completed the paperwork, a task that researchers estimated would take about 10 minutes.
Luby's team found that parents living in poverty appeared more stressed and less able to nurture their children during that exercise. In cases where poor parents were rated as good nurturers, the children were less likely to exhibit the same anatomical changes in the brain as poor children with less nurturing parents.
"Parents can be less emotionally responsive for a whole host of reasons," Luby said. "They may work two jobs or regularly find themselves trying to scrounge together money for food. Perhaps they live in an unsafe environment. They may be facing many stresses, and some don't have the capacity to invest in supportive parenting as much as parents who don't have to live in the midst of those adverse circumstances."
The researchers also found that poorer children were more likely to experience stressful life events, which can influence brain development. Anything from moving to a new house to changing schools to having parents who fight regularly to the death of a loved one is considered a stressful life event.
Luby believes this study could provide policymakers with at least a partial answer to the question of what it is about poverty that can be so detrimental to a child's long-term developmental outcome. Because it appears that a nurturing parent or caregiver may prevent some of the changes in brain anatomy that this study identified, Luby said it is vital that society invest in public health prevention programs that target parental nurturing skills. She suggested that a key next step would be to determine if there are sensitive developmental periods when interventions with parents might have the most powerful impact.
"Children who experience positive caregiver support don't necessarily experience the developmental, cognitive and emotional problems that can affect children who don't receive as much nurturing, and that is tremendously important," Luby said. "This study gives us a feasible, tangible target with the suggestion that early interventions that focus on parenting may provide a tremendous payoff." Aspira Continuing Education Online Courses
###
Funding for this research comes from the National Institute of Mental Health (NIMH) of the National Institutes of Health (NIH).
NIH grant numbers 2R01 MH064769-06A1, PA-07-070 NIMH R01 and 5K01 MH090515-04.
Luby J, Belden A, Botteron K, Marrus N, Harms MP, Babb C, Nishino T, Barch D. The effects of poverty on childhood brain development: The mediating effect of caregiving and stressful life events. JAMA Pediatrics vol. 167 (11), November 2013, published online Oct. 28, 2013. http://archpedi.jamanetwork.com/journal.aspx
Washington University School of Medicine's 2,100 employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children's hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked sixth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children's hospitals, the School of Medicine is linked to BJC HealthCare.
October 22, 2013
Research uncovers new details about brain anatomy and language in young children
PROVIDENCE, R.I. [Brown University] — Researchers from Brown University and King's College London have gained surprising new insights into how brain anatomy influences language acquisition in young children.
Their study, published in the Journal of Neuroscience, found that the explosion of language acquisition that typically occurs in children between 2 and 4 years old is not reflected in substantial changes in brain asymmetry. Structures that support language ability tend to be localized on the left side of the brain. For that reason, the researchers expected to see more myelin — the fatty material that insulates nerve fibers and helps electrical signals zip around the brain — developing on the left side in children entering the critical period of language acquisition. But that is not what the research showed.
"What we actually saw was that the asymmetry of myelin was there right from the beginning, even in the youngest children in the study, around the age of 1," said the study's lead author, Jonathan O'Muircheartaigh, the Sir Henry Wellcome Postdoctoral Fellow at King's College London. "Rather than increasing, those asymmetries remained pretty constant over time."
That finding, the researchers say, underscores the importance of environment during this critical period for language.
O'Muircheartaigh is currently working in Brown University's Advanced Baby Imaging Lab. The lab uses a specialized MRI technique to look at the formation of myelin in babies and toddlers. Babies are born with little myelin, but its growth accelerates rapidly in the first few years of life.
The researchers imaged the brains of 108 children between ages 1 and 6, looking for myelin growth in and around areas of the brain known to support language.
While asymmetry in myelin remained constant over time, the relationship between specific asymmetries and language ability did change, the study found. To investigate that relationship, the researchers compared the brain scans to a battery of language tests given to each child in the study. The comparison showed that asymmetries in different parts of the brain appear to predict language ability at different ages.
"Regions of the brain that weren't important to successful language in toddlers became more important in older children, about the time they start school," O'Muircheartaigh said. "As language becomes more complex and children become more proficient, it seems as if they use different regions of the brain to support it."
Interestingly, the association between asymmetry and language was generally weakest during the critical language period.
"We found that between the ages of 2 and 4, myelin asymmetry doesn't predict language very well," O'Muircheartaigh said. "So if it's not a child's brain anatomy predicting their language skills, it suggests their environment might be more influential."
The researchers hope this study will provide a helpful baseline for future research aimed at pinpointing brain structures that might predict developmental disorders.
"Disorders like autism, dyslexia, and ADHD all have specific deficits in language ability," O'Muircheartaigh said. "Before we do studies looking at abnormalities we need to know how typical children develop. That's what this study is about."
"This work is important, as it is the first to investigate the relationship between brain structure and language across early childhood and demonstrate how this relationship changes with age," said Sean Deoni, assistant professor of engineering, who oversees the Advanced Baby Imaging Lab. "The study highlights the advantage of collaborative work, combining expertise in pediatric imaging at Brown and neuropsychology from the King's College London Institute of Psychiatry, making this work possible."
###
Other authors on the paper include Douglas Dean, Holly Dirks, Nicole Waskiewicz, and Katie Lehman from Brown's Baby Imaging Lab, and Beth Jerskey from Brown's Alpert Medical School. The work was funded by the National Institutes of Mental Health and the Wellcome Trust.
Editors: Brown University has a fiber link television studio available for domestic and international live and taped interviews, and maintains an ISDN line for radio interviews. For more information, call (401) 863-2476 ASW Continuing Education
--------------------------------------------------------------------------------
[ Back to EurekAlert! ] [ Print | E-mail Share Share ] [ Close Window ]
AAAS and EurekAlert! are not responsible for the accuracy of news releases posted to EurekAlert! by contributing institutions or for the use of any information through the EurekAlert! system.
HOME DISCLAIMER PRIVACY POLICY TERMS & CONDITIONS CONTACT US TOP
Copyright ©2013 by AAAS, the science society.
Labels:
anatomy,
asw continuing education,
brain,
language,
neuropsychology,
neuroscience,
research
October 20, 2013
NIMH Grantee Receives 2013 Nobel Prize
Congratulations to current NIMH grantee Thomas C. Südhof, M.D., at Stanford University School of Medicine, for winning the Nobel Prize in Physiology or Medicine for his work on how the brain sends and receives chemical messages.
Thomas C. Südhof, M.D.
Thomas C. Südhof, M.D.
Stanford University
School of Medicine
“We are extremely proud of Dr. Südhof,” said National Institute of Mental Health (NIMH) Director Thomas Insel, M.D. “NIMH has supported Dr. Südhof's ground-breaking research for more than two decades as part of our commitment to understanding the fundamental mechanisms of brain function."
The human brain houses about 100 billion neurons—about half the number of stars in the Milky Way. Each of these neurons “converses” with, on average, thousands of other neurons, sending molecular messages in a matter of milliseconds, about the same timeframe as a camera flash. How these messages are sent in such a rapid and precise manner has long been a mystery to neuroscientists. When these messages go awry, mental disorders such as schizophrenia, autism, and depression may arise.
Specifically, Dr. Südhof parsed the proteins that are used in a synapse—the gap between neurons where one neuron reaches out to talk to another via chemical messengers known as neurotransmitters. These specialized spaces are comprised of three components: the messenger or presynaptic neuron, the recipient or postsynaptic neuron, and the cleft or space between these two neurons. Dr. Südhof’s work identified key molecules involved in the rapid release of neurotransmitters from the terminals of presynaptic neurons and revealed how electrical signals in the form of calcium ions instruct a protein called synaptotagmin. Once calcium binds to synaptotagmin, the protein serves as a switch for neurotransmitter-carrying cellular shuttles called vesicles to fuse with the outer surface of the presynaptic neuron and release these chemical messengers into the synaptic cleft. Upon release, the neurotransmitters cross the synaptic cleft and bind to docking sites or receptors on the postsynaptic neuron, triggering an electrical signal to pulse through it. Südhof’s work revealed that synaptotagmins also act as universal calcium sensors in non-neuronal cells, functioning, for example, in the release of hormones such as insulin from pancreatic beta cells.
Dr. Südhof shares the world’s most prestigious science award with James E. Rothman, Ph.D., at Yale University, and Randy W. Schekman, Ph.D., at the University of California, Berkeley. Dr. Rothman unraveled protein machinery that allows vesicles to fuse with their targets to permit transfer of cargo. Dr. Schekman discovered a set of genes that were required for vesicle traffic. The researchers will share a prize that totals roughly $1.2 million USD.
Previously, Dr. Südhof and Richard H. Scheller, Ph.D., at Genentech, collected the 2013 Albert Lasker Basic Medical Research Award for their work. Known as “America’s Nobels,” the Lasker Awards often predict future Nobel Prize recipients.
The National Institutes of Health (NIH) has supported Dr. Südhof’s research over the past 22 years. In turn, Dr. Südhof has served on several study sections at the NIH Center for Scientific Review, in addition to the Molecular, Cellular, and Developmental Neuroscience study section at NIMH. Over the years, Dr. Südhof’s work on the neurotransmitter release machinery has been supported with research program grants as well as center grants from NIMH. He is also the recipient of an NIMH MERIT (Method to Extend Research in Time) award, which along with an additional NIMH grant and funding from the Howard Hughes Medical Institute helped support his Nobel work. MERIT awards provide up to 10 years of stable research support for highly productive outstanding investigators working on projects well aligned with the mission of NIMH Social Worker Continuing Education
Dr. Südof also holds an NIH TR01 award for work to facilitate the creation of neurons from non-neuronal cells (skin fibroblasts of human patients). This work is anticipated to provide a novel way for scientists to study the biological effects of gene mutations associated with neuropsychiatric diseases
October 19, 2013
PBS Documentary “Brains on Trial”
A convenience store robbery goes horribly wrong: A teenager high on cocaine stands trial for attempted murder.
Brains on Trial PBS documentaryUsing this fictional crime, a two-episode PBS program titled “Brains on Trial” explores the brains of the key courtroom players—defendant, witnesses, jurors, and judge. Is a witness lying or telling the truth? How can two people see the same event and yet remember it so differently? These and other questions are what neuroscience currently is being asked to do using brain scans.
Join host Alan Alda as he visits and conducts brain scan experiments with neuroscientists, such as the National Institute of Mental Health (NIMH)’s Jay Giedd, M.D., in the quest to answer how brain research can influence and reform the criminal justice system. Dr. Giedd is chief of the Unit on Brain Imaging in the Child Psychiatry Branch at NIMH LCSW Continuing Education
Labels:
brain,
brains,
lcsw continuing education,
remember,
truth
September 02, 2013
The More Hemispheric Lateralization, the Better Thinking Performance
By examining activity of the living human brain at rest via fMRI, NIMH intramural scientists have discovered a secret to how it enhances thinking ability. It turns out that left brain regions are biased to talk more to each other, while right brain regions talk more evenly with both hemispheres. These biases are most pronounced in brain regions associated with the specialized functions of the two hemispheres – e.g., language and motor control on the left and visual/spatial attention on the right. Such lateralization is associated with enhanced cognition, say Drs. Stephen Gotts, Hang Joon Jo, Alex Martin, and colleagues of the NIMH Cognitive Neuropsychology Section, Laboratory of Brain and Cognition. The more such lateral specialization subjects showed at rest, the better they performed on verbal and spatial tasks later.
For more information, see PNAS Blog: Brain Halves Interact Differently with Each Other CBT - How to Implement Trauma-Focused Cognitive Behavioral Therapy
Two types of lateralization
Reference
Two distinct forms of functional lateralization in the human brain. Gotts SJ, Jo HJ, Wallace GL, Saad ZS, Cox RW, Martin A. Proc Natl Acad Sci U S A. 2013 Aug 19. [Epub ahead of print] PMID: 23959883
June 19, 2013
Bullying Exerts Psychiatric Effects into Adulthood
Once considered a childhood rite of passage, bullying lingers well into adulthood. Bullies and victims alike are at risk for psychiatric problems such as anxiety, depression, substance abuse, and suicide when they become adults, reported a study partially funded by the National Institute of Mental Health (NIMH) that was published in the April issue of JAMA Psychiatry.
Background
Bullying is a repetitive, aggressive act done to abuse or intimidate others. It can take on various forms—primarily verbal, emotional, and physical, although cyberbullying is also on the rise. Typically these scenes occur inside school or on the playground, but they can also happen at home or at work. A power imbalance usually is involved in which one child or a group of children torments another child who is considered “weaker.” Methods employed by bullies include threats, rumor-spreading, and exclusion.
Most of what experts know about the effects of bullying comes from short-term observational studies. These studies reflect general society’s view that most people overcome these events by the time they become adults.
“Initially I too was skeptical about these long-term effects,” says study author William Copeland, Ph.D., at Duke University, who as an epidemiologist knew of other traumatic events that do not linger psychologically, such as maltreatment and physical abuse. “Yet this is something that stays with people. A large number of people express lasting effects decades after their childhood experiences.”
Copeland and his colleagues tapped into a local population sample of 1,420 children from 11 Western North Carolina counties. Starting at the ages of 9, 11, and 13, the kids, along with their parents, were interviewed annually until the age of 16, fielding questions about peer relations and home and community settings. The participating children were again interviewed at 19, 21, and 24 to 26 years of age. Four groups emerged from this longitudinal study: people who were never involved in bullying, people who were victims, people who were bullies, and people who were both.
Results of the Study
More than half of the study’s youth reported being neither a bully nor a victim. Around a quarter of the study group claimed that they were victimized. About 7 percent confessed to being a bully. A similar percentage said that they were both, a group the researchers labeled as “bully-victims.”
Compared to those who went through childhood unscathed, victims had four times the prevalence of agoraphobia, generalized anxiety, and panic disorder when they became adults. Overall, bullies had four times the risk of developing antisocial personality disorder. These disorders still stood even after other factors were taken into account, such as preexisting psychiatric problems or family hardships.
Bully-victims fared the worst. Also known as “loners,” these individuals start out with less developed social skills and are seen as more impulsive and aggressive. When picked on, they respond by picking on others. Their numbers, compared to those never involved in bullying, tell the story: 14 times the risk of panic disorder, 5 times the risk of depressive disorders, and 10 times the risk of suicidal thoughts and behavior.
“Victims report the greatest anxiety problems. They might become successful people later on, but they still think about the event and hold onto it. Bullies are socially adept and may find ways in adulthood to use these skills in a pro-social manner. Folks really underestimate who are the bully-victims. These are the ones who end up having the most significant emotional problems including suicidality,” explained Copeland, who is also a father of two Social Worker Continuing Education
Significance
All these disorders impart a great emotional and financial cost to society. Lowering and/or preventing bullying could possibly reduce human suffering and long-term health costs—not to mention creating a safer environment for children to grow up in.
Research into resilience or why some are able to bounce back in adulthood is ongoing. Some key molecules and brain circuit pathways have been identified in animals. Other research areas under exploration include physiology, genetics, epigenetics, and cognitive therapies.
What’s Next
Studies looking into which interventions work best for bullying are underway. Once these interventions are identified, research is needed to see at what stages in life they should they be administered. Lastly, other factors that play a role in bullying and victimization, such as sexual orientation, need exploration.
“This study suggests that we should pay attention to what’s going on between peers,” said Copeland, adding that kids spend more time each day with their peers, including school and online, than with their parents. “What happens to kids when they’re with their peers is as important, or may be more important, than what happens at home,” said Copeland.
Reference
Copeland WE, Wolke D, Angold A, Costello EJ. Adult Psychiatric Outcomes of Bullying and Being Bullied by Peers in Childhood and Adolescence. JAMA Psychiatry, published April 2013.
Grant number: K23 MH080230
Subscribe to:
Posts (Atom)